Stereotactic TransperinealProstate biopsy-STPB
Diagnose quickly and accurately with little discomfort.
About Prostate Cancer
Stereotactic Transperineal Prostate biopsy - STPB
According to the American Cancer Society, 1 in 7 men will be diagnosed with prostate cancer in their lifetime. Most of these diagnoses are made with a standard transrectal biopsy administered in the office by urologists. However, often times a patient will have a continued rising PSA, despite having had a negative office biopsy. This causes anxiety for patients and physicians. Fortunately, Chicago Prostate Center has developed Stereotactic Transperineal Prostate biopsy or STPB. This is the most comprehensive, sophisticated prostate biopsy technique available, diagnosing 40% more cancer than the standard office procedure—cancer that would have otherwise gone undetected.
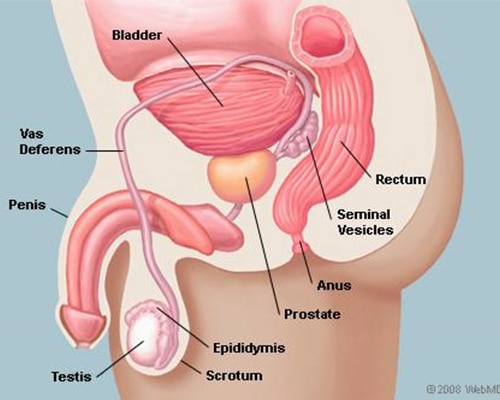
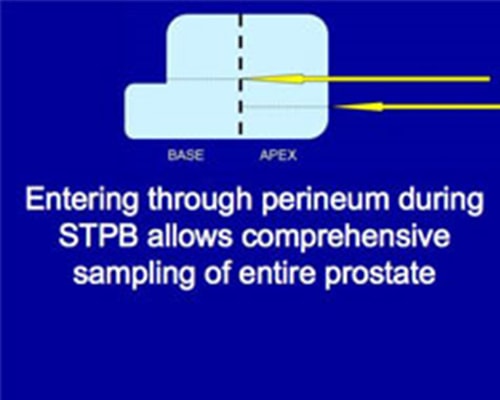
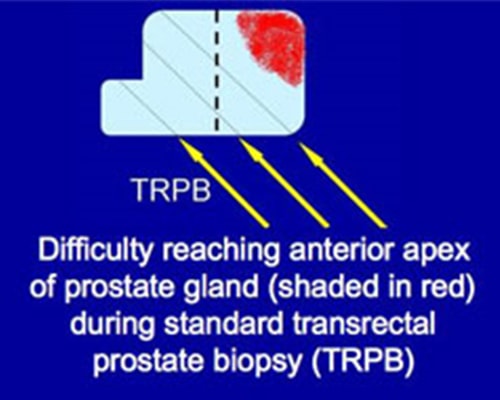
Many of the cancers missed by the standard transrectal biopsy are in the apex of the prostate gland. The apex of the prostate gland is located at the bottom of the gland. The apex is pointed down to the Perineum as opposed to the base which is wider and located next to the bladder.
Although we have found cancer throughout the prostate using STPB, there is significantly a higher rate in the apex, and more specifically, the anterior apex of the prostate. This may suggest that transrectal needle guidance may be missing the apex of the prostate, however, with a transperineal approach, the apex is easily reached. Therefore, more and more patients are choosing this option as their first choice for prostate biopsy.
Benefits of STPB
- Diagnosing 40% more cancer
- One-time, out-patient procedure (no hospital stay needed)
- Minimally invasive (no incisions or stitches)
- Performed under general anesthesia with no discomfort
- Infection rate negligible
- Confidence in exact location of cancer
- Minimal, if any, post-operative pain
- Return to normal activity within a day
STPB is performed by taking an average of 40 samples of the prostate through the Perineum while the patient is under general anesthesia. Performed as an outpatient procedure, it allows more comprehensive sampling, compared to the transrectal method, which takes fewer samples through the rectum. Unlike random sampling with transrectal prostate biopsy, with our extensive template-guided approach, we are able to identify exactly where the positive and negative specimens were retrieved. This allows for more sophisticated treatment plans for those with positive biopsies, and relief for those patients whose biopsies were negative.
Because specimens are obtained through the rectum (where large amounts of bacteria are present) for standard transrectal office biopsy, urologic complications including bacteria in the urine, urinary tract infection (UTI), bacteria in the blood, fever episodes, and sepsis (pathogenic microorganisms or their toxins in the blood) can occur in about 3% of patients1-2. These serious infections after transrectal biopsy are often resistant to antibiotics and require hospitalization, leading to death in 1/1000 men2. During STPB, the prostate specimens are obtained through the Perineum and therefore, we have not seen any infection.
Our patients often tell us how grateful they are for giving them peace of mind with regards to whether or not they have prostate cancer. Finally, STPB is covered by most insurance plans, including Medicare.
If you have had a rising PSA or abnormal digital rectal exam, call us today at 630.248.0717 to find out more.
- Zaytoun OM, Vargo EH, Rajan R et al. Emergence of fluoroquinolone-resistant Escherichia coli as cause of postprostate biopsy infection: Implications for prophylaxis and treatment. Urology, May 2011, Vol 77(5), 1035-1041.
- Nam RK, Saskin R, Lee Y et al. Increasing hospital admission rates for urologic complications after transrectal ultrasound guided prostate biopsy. Journal of Urology, March 2010, Vol 183, 963-969.